Ankle Foot Orthoses (AFOs)
Introduction
Orthosis:
- “an externally applied device that is designed and fitted to the body”. (The Australian Orthotic Prosthetic Association, 2017)
- Can be prefabricated or custom made
Orthotics:
- “A branch of mechanical and medical science that deals with the design and fitting of” orthoses. (Mirriam-Webster, 2017)
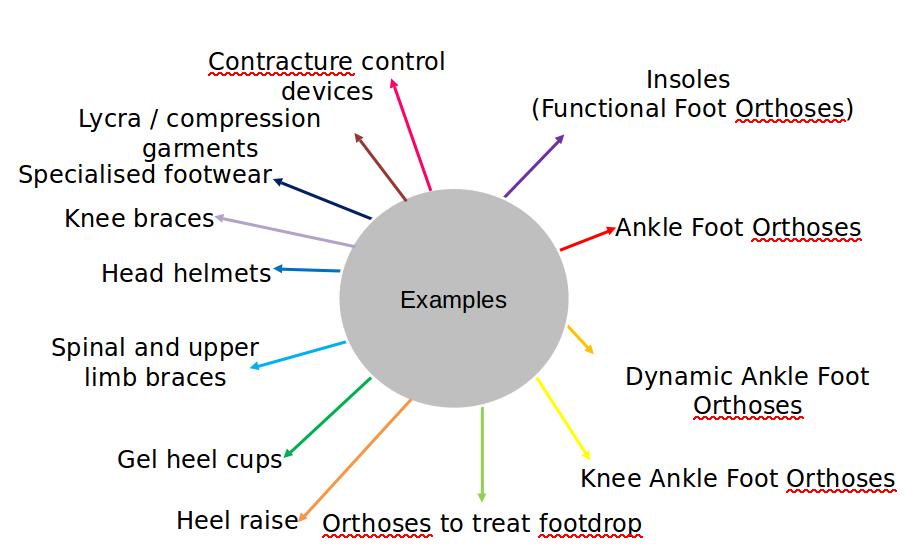
Examples of Different Orthoses:
Ankle Foot Orthoses (AFOs)
What are they?
- Brace worn on the lower leg that extends from under the foot to below the knee.
- Custom or pre-fabricated - different designs and materials.
- Immobilises or limits movement at the ankle.
Purpose
- Lower limb pain relief
- Prevent joint and muscle changes
- Provide a more stable base of support
- To manipulate the position of the ground reaction
- To stretch the leg muscles (usually the gastrocnemius)
How can AFOs vary?
Different materials (e.g.polypropylene, carbon fibre, silicone)
- Weight
- Strength / resistance
- Durability
- Ease of which it can be adjusted
- Comfort
Different designs
- Amount of material (leafspring) / trimlines
- Length (met heads)
- Angle of the ankle
- Position of the shank
- Hinge / amount of movement allowed
Different designs of footwear
- Consideration of the Ankle Foot Orthoses Footwear Combination (AFOFC) is very important – a shoe can partly change the effect of an AFO.
Advantages/Disadvantages of Ankle Foot Orthoses
| Advantages | Disadvantages |
|---|---|
| Improved Function | Muscle weakness |
| Reduce Pain | Loss of sensation |
| Prevent Joint and muscle changes | More medical appointments |
| Increase Stability | Decreased Compliance |
AFO Usage
In the UK, AFO prescription is:
- widespread.
- diverse.
- not confined to a particular patient group.
- not entirely prescriptive (consensus varies).
- conducted by different professions e.g orthotists/physios.
Clinics may:
- be located within the NHS and private practice.(NHS services are usually commissioned).
- involve multidisciplinary working.
Which AFO design suits which clinical population?
AFO design depends on the individual presentation and not the medical condition that an individual has been diagnosed with.
In order to ascertain whether an individual may benefit from an AFO, the goal must first be decided and any potential drawbacks considered.
In order to realise the goal, a clinical examination must be carried out (+/- other tests such as patient questionnaires, gait analysis).
AFO’s should not be prescribed without considering and collecting outcome measures. The purpose of outcome measures is to measure whether the goal is likely to be achieved but outcome measures can also be used to check that there are no detrimental effects.
One type of prescription does not fit all!
Possible Outcome Measures
- Reduce progression of deformity/Maintain range of motion
- Photographs
- Physical examination measures
- Foot assessments eg Foot Posture Index
- Improve gait
- Clinical video
- Clinical video plus observational gait measure eg Edinburgh Gait Score
- Videovector
- Fully instrumented (3D)
- Improve function
- Timed up and go
- 6 minute walk test
- Walking speed
- Gross Motor Function Measure
- Patient questionnaires
- Balance
- Single leg stance
- Star excursion balance test
- Berg balance scale
- Decrease pain
- Patient questionnaires
- Visual analogue scale
What is the state of scientific evidence with regards to AFOs?
This depends on the goal and the patient population … An example:
Systematic reviews / meta analyses - Use of AFOs in children with Cerebral Palsy - Children with cerebral palsy using ankle-foot orthoses have improved stride length and dorsiflexion angle during gait in a pooled meta-analyses of cohort studies and clinical trials (Betancourt et al., 2019)
- Children with cerebral palsy using AFOs have improved gait and motor function (Lindaf et al., 2019)
- AFOs improved ankle and knee range of motion, walking speed and stride length (Pourhosseingholi et al., 2019)
- The Gait Deviation Index (GDI), ankle Gait Variable Score, knee Gait Variable Score, nondimensional speed,and nondimensional step length do not change in children with cerebral palsy who wear AFOs. Only step length shows a significant difference between barefoot and AFO conditions (Ries et al., 2015)
Why is there not always consensus within the evidence base?
| Considerations prior to prescription | Considerations with the AFO prescription |
|---|---|
| What is the patient’s muscle length? | Angle of the ankle |
| What is the patient’s range of motion? | Rigidity of the AFO |
| Does the patient have an emerging foot deformity? | Design to support the foot |
| Is the patient at risk of foot deformity? | Shank inclination |
| Does the patient have increased muscle tone such as spasticity? | Shoe design |
| Does the patient have a leg length discrepancy? | Flexibility of ankle dorsiflexion and plantarflexion |
| Is the patient’s problem bilateral? | Do leg lengths need to be equalised? |
| (Considerations in relation to the drawbacks) | Trimlines in relation to the metatarsal heads |
| Position and design of straps |
A focus on using AFO’s to improve gait
Most complex area of AFO provision is the manipulation of the position of the ground reaction in relation to the joints of the lower limb
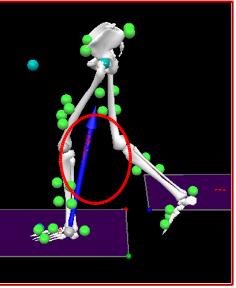
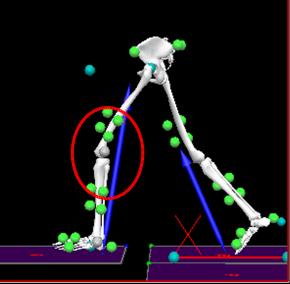
When AFOs are used to improve gait, they work on the principle of facilitating best alignment of the ground reaction.
The forces and moments acting within and on the body cause it to move in the way it does.
The ground reaction (measured by a force plate) is the force that the ground produces when any person or object makes contact with it.
When a force is applied some distance away from a joint it will rotate the joint in the direction of the force – this is called the joint moment (Kirtley, 2006).
The ground reaction produces an external joint moment which must be matched by an internal joint moment (usually produced by muscles).
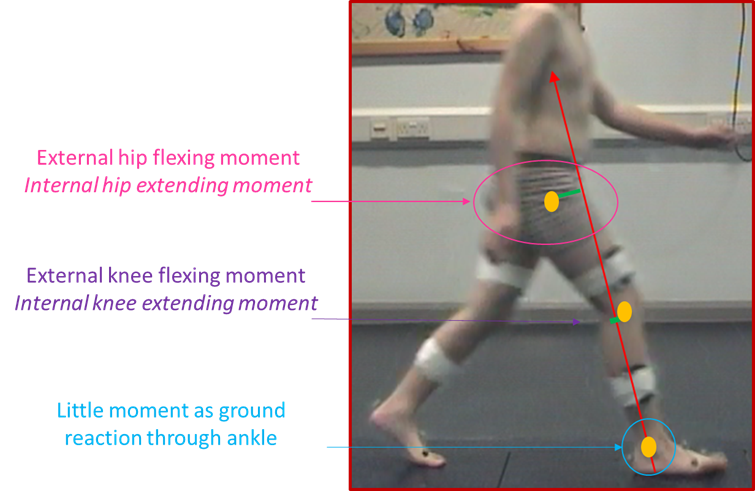
The further the ground reaction is away from the joint, the larger the moment (and the larger the turning force applied to the joint).
In healthy walking, most of the time external moments are kept small (and therefore internal moments are small).
During video vector assessment, the GR (which is overlaid onto the video) is compared to typical GR positions at set points in the gait cycle.
As a clinician or researcher, it is important to have an understanding of the normal alignment of the ground reaction (beyond the scope of this session).
- Ground reaction further behind the knee
- Larger external knee flexing moment
- Larger internal knee extending moment
- Knee extensor / calf muscles have to work harder to prevent the knee from flexing further
- Consequences
- Efficiency
- Other joints
- Future
The OSKAR Approach
The Optimal Segmental Kinematic Alignment approach to Rehabilitation (OSKAR) is an orthotic method of treating children with lower limb neuromuscular conditions originally developed by Elaine Owen, a world renowned physiotherapist who was awarded an MBE in 2012 for services to children with disability.
OSKAR incorporates a holistic view of the child to plan orthotic and physiotherapy treatments which are goal orientated and reviewed regularly.
The International Classification of Functioning (ICF) is used as a tool to guide goal choice and outcomes.
The ICF is a framework developed by the World Health Organization used to define and measure the health and functioning of children up to age 18 years by describing the consequences of a health condition in terms of body function and structures, activity, and participation. It also takes into account the social aspect of the child’s functioning.
The ethos of OSKAR is based on the key principle of biomechanical optimisation of the AFOFC – the process of designing, aligning and tuning an orthosis to maximise it’s performance for a given task (tuning refers to the fine adjustments that are made when the activity is assessed).
Conclusions
AFOs:
- are complicated and their prescription can vary tremendously.
- the advantages of prescribing AFOs must be clearly considered alongside the drawbacks.
AFO prescription should:
- take into consideration the patient presentation (clinical assessment and other tests) and the design of the AFO.
- be goal driven.
- measure the effect on the goal using appropriate outcome measures including those that also monitor the effect on quality of life.
AFO research should:
- be clear as to the specific question being asked.
- provide as much information about the AFO as possible.
- recognise and start to address the effect of specific design features on specific aspects of gait.
References
Aboutorabi, A. et al. (2017). Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Annals of Physical and Rehabilitation Medicine, 60, 393–402. doi.org/10.1016/j.rehab.2017.05.004
Betancourt, J.P., Eleeh, P., Stark, S. & Jain, N.B. (2019). Impact of Ankle-Foot Orthosis on Gait Efficiency in Ambulatory Children With Cerebral Palsy A Systematic Review and Meta-analysis. American Journal of Physical Medicine & Rehabilitation, 98 (9), 759-770.
Bettoni, E., Ferriero, G., Bakhsh, H., Bravini, E., Massazza, G., & Franchignoni, F. (2016). A systematic review of questionnaires to assess patient satisfaction with limb orthoses. Prosthetics & Orthotics International, 40(2) 158–169.
doi: 10.1177⁄0309364614556836Eddison, N., Mulholland, M., & Chockalingam, N. (2017). Do research papers provide enough information on design and material used in ankle foot orthoses for children with cerebral palsy? A systematic review. Journal of Children’s Orthopaedics, 11, 263-271. doi: 10.1302⁄1863-2548.11.160256
Firouzeh, P., Sonnenberg, L.K., Morris, C., & PritchardWiart, L. (2019). Ankle foot orthoses for young children with cerebral palsy: a scoping review. Disability and Rehabilitation, https://doi.org/10.1080/09638288.2019.1631394.
Harlaar et al. (2010). Studies examining the efficacy of Ankle Foot Orthoses should report activity level and mechanical evidence. Prosthetics & Orthotics International, 34(3), 327-335. doi: 10.3109⁄03093646.2010.504977
Lintanf, M. et al. (2018). Effect of ankle-foot orthoses on gait, balance and gross motor function in children with cerebral palsy: a systematic review and meta-analysis. Clinical Rehabilitation, 32(9), 1175-1188. Clinical Rehabilitation. Doi: 10.1177⁄0269215518771824
McCaughan et al. (2019). Orthotic management of instability of the knee related to neuromuscular and central nervous system disorders: qualitative interview study of patient perspectives. BMJ Open, 9(10), doi.org/10.1136/bmjopen-2019-029313.
Mirriam-Webster dictionary. (2017). Retrieved 12th October , 2017, from https://www.merriam-webster.com/dictionary/orthotics
Phillips, M., Radford, K., & Wills, A. (2011). Ankle foot orthoses for people with Charcot Marie Tooth disease – views of users and orthotists on important aspects of use. Disability and rehabilitation, 6(6), 49-499. doi: 10.3109⁄17483107.2010.549899
Rahlin, M. (2016). Physical therapy for children with cerebral palsy An evidence based approach. Thorofare: Slack Inc.
Ries, A.J., Novacheck, T., & Schwartz, M. (2015). The Efficacy of Ankle-Foot Orthoses on Improving the Gait of Children With Diplegic Cerebral Palsy: A Multiple Outcome Analysis. PM&R, 7(9), 922-929. doi: 10.1016/j.pmrj.2015.03.005
The Australian Orthotic Prosthetic Association. (2017). Retrieved 12th October, 2017, from https://www.aopa.org.au/careers/what-are-orthoses-and-prostheses
World Health Organization. (2019). International Classification of Functioning, Disability and Health (ICF). Retrieved from https://www.who.int/classifications/icf/en/