Lateral Ankle Sprains
Introduction
Lateral Ankle Sprains
- Common during landing, deceleration, change of direction
- Court and field sports e.g. tennis, basketball, netball, football etc.
Studied Example 1
Fong et al. (2009)
- Case report – accidental injury:
- Inversion = 48°
- Internal rotation = 10°
- Ankle DF rather than PF
Studied Example 2
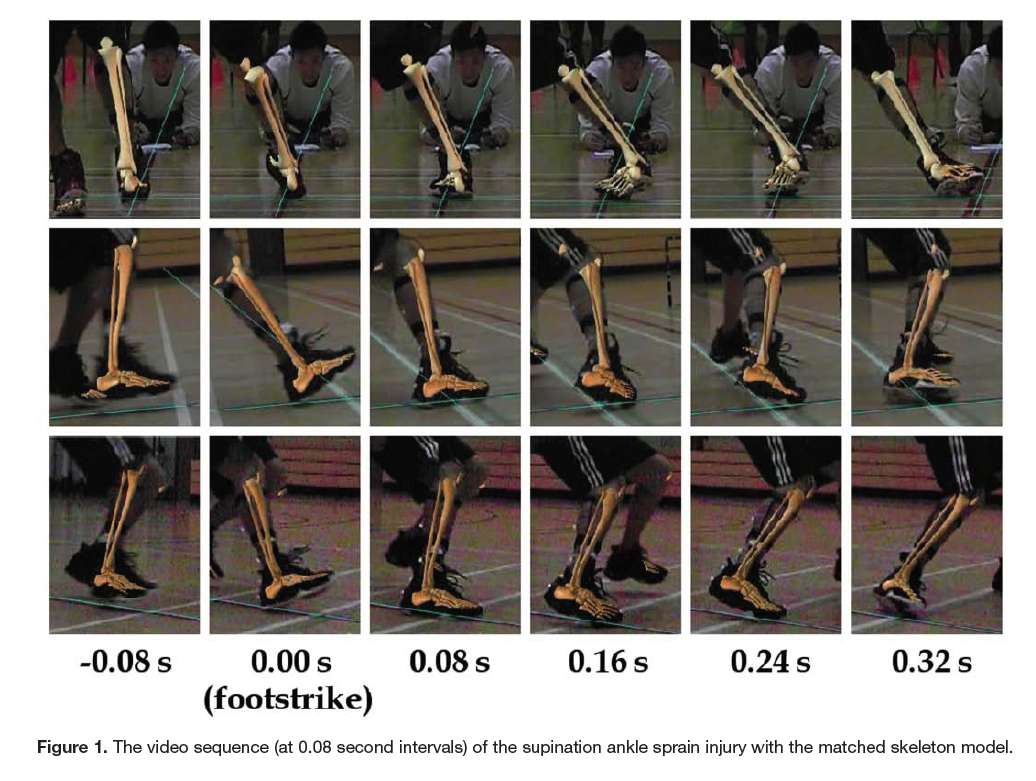
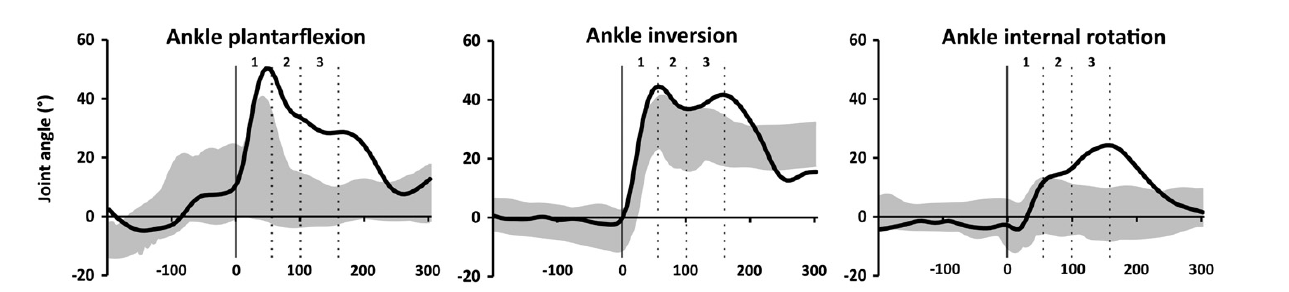
Gehring et al. (2013)
3D motion capture of accidental ankle sprain:
Rapid increase: - Plantar flexion (1240°/s) - Inversion (1290 °/s) - Internal rotation (580 °/s)
Studied Example 3
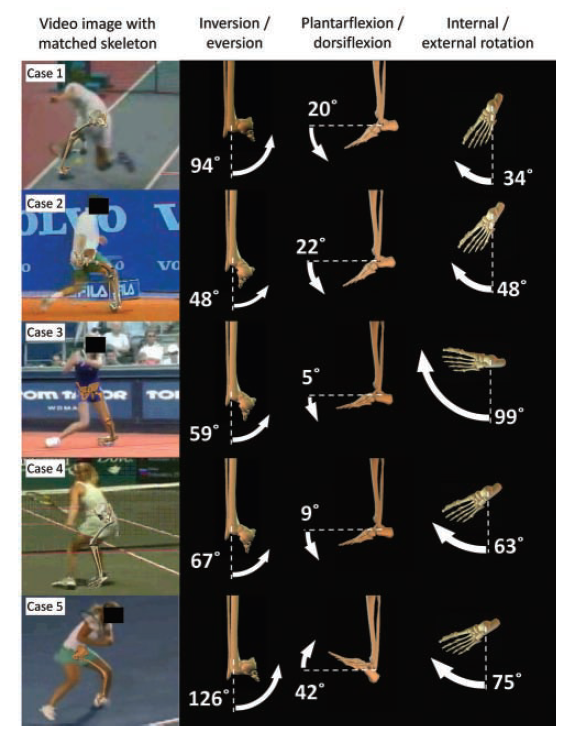
Fong et al. (2012)
Televised ankle sprains in tennis:
- Model-based image matching approach to understand real time
- Sampling frequency – 25 – 50 Hz
- Large variation in motions resulting in the sprain
- Mechanism likely a result of type of movement
Definition of Ankle Sprain
Gribble et al. (2016) International Ankle Consortium (IAC) consensus
“An acute traumatic injury to the lateral ligament complex of the ankle joint as a result of excessive inversion of the rear foot or a combined plantar flexion and adduction of the foot”
Prevalence and Consequences
Prevalence
How many have had a sprain?
- 15% of all injuries are ankle sprains (Hootman et al., 2007)
- 7 ankle sprains per 1000 exposures (Doherty et al., 2014)
- 3 – 5% of all A&E presentations are for ankle sprains (UK) (Cooke et al., 2003; Lamb et al., 2009)
Consequences
- Swelling
- Pain
- Can’t put pressure on it
Ankle Anatomy
| Structure | Position | Function | Notes |
|---|---|---|---|
| ATFL | Anterior edge of the lateral malleolus of the fibular Runs horizontally forward and downward and attaches to the neck of the talus, in front of the lateral malleolar facet | Limits: Anterior displacement and medial shifting of the talus Posterior displacement and lateral rotation of the tibia and fibula, primarily in PF. Also prevents lateral talar tilt. | Short ligament, widens slightly from top to bottom |
| CFL | Originates from the anterior part of LM, often with a partial connection to ATFL at the fibula just distal to the ATFL It runs posteromedially, downward and backward, to be inserted into the calcaneus, distal to the subtalar joint. The insertion location on calcaneus is highly variable The fibres of the CFL pass through both the subtalar and ankle joints | CFL stretches and comes under strain in the dorsiflexion position Responsible for resistance against inversion and internal rotation stress | Strong flat oval or cord-like structure Thicker and stronger than ATFL |
Key Point
ATFL = most vulnerable and main ligament affected
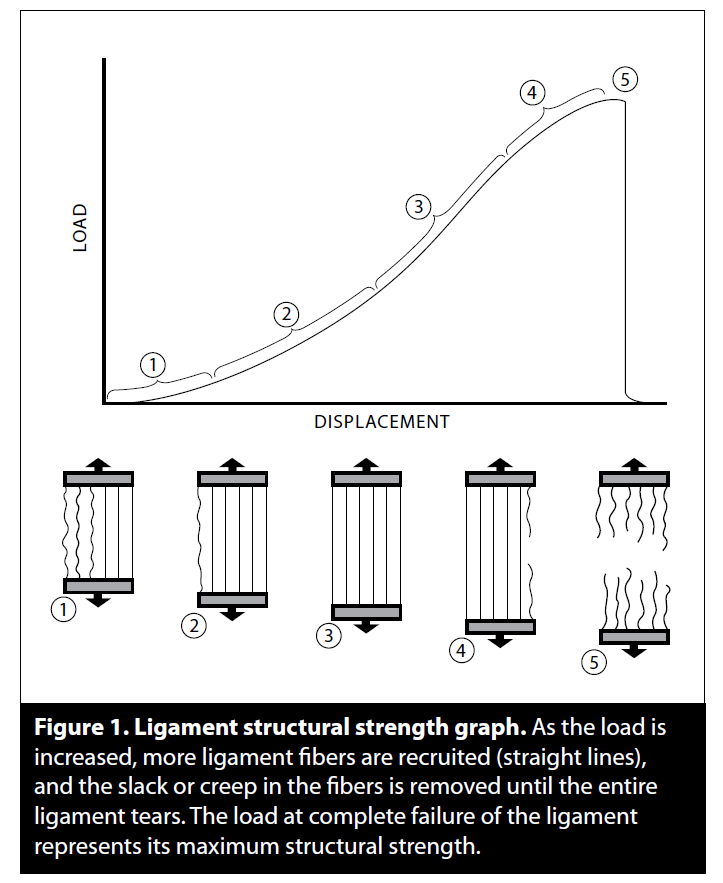
Ligament Structural Strength
Hauser & Dolan (2011)
- Toe region
- Uncrimping/ elongation
- Nearly linear elongation
- Microdamage/ plastic region
- Complete failure
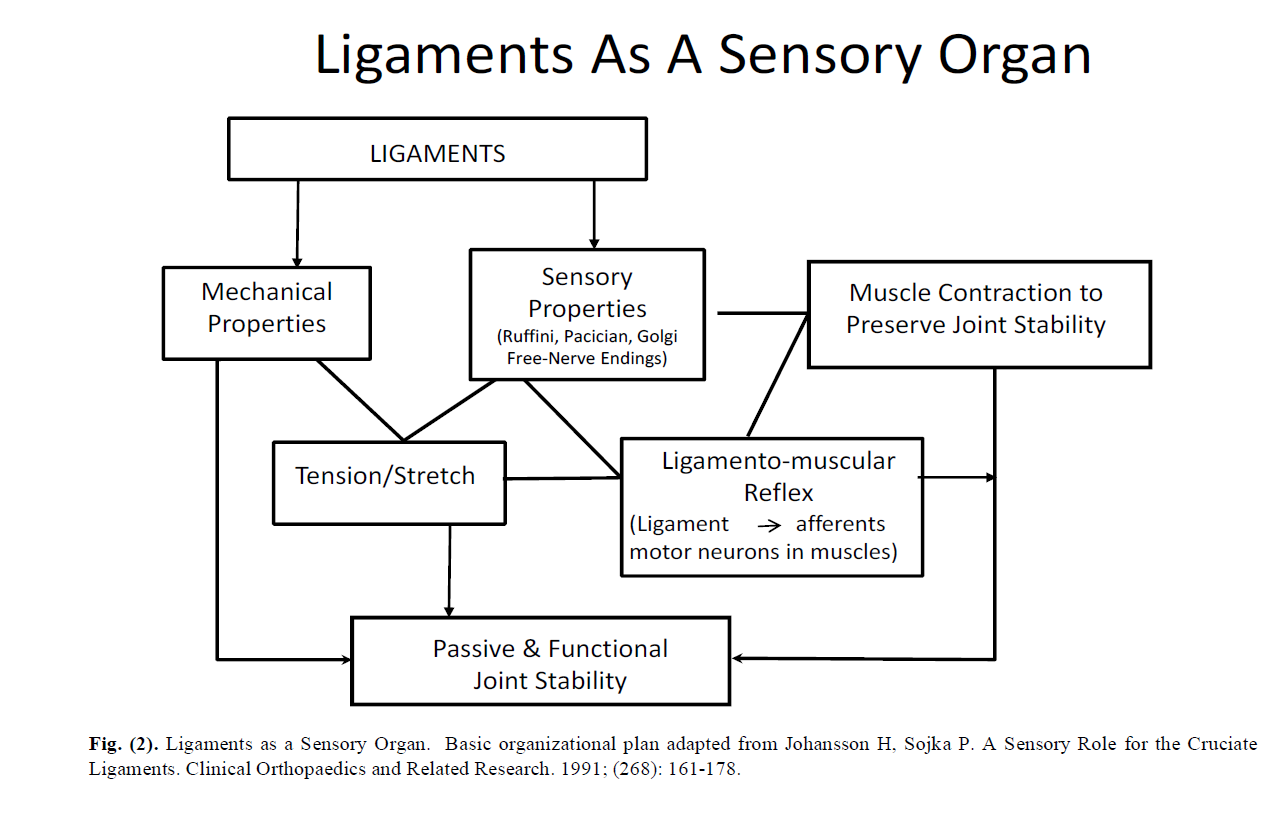
Ligaments as a Sensory Organ
Hauser and Dolan (2011)
Ligament Healing
Phases of Healing
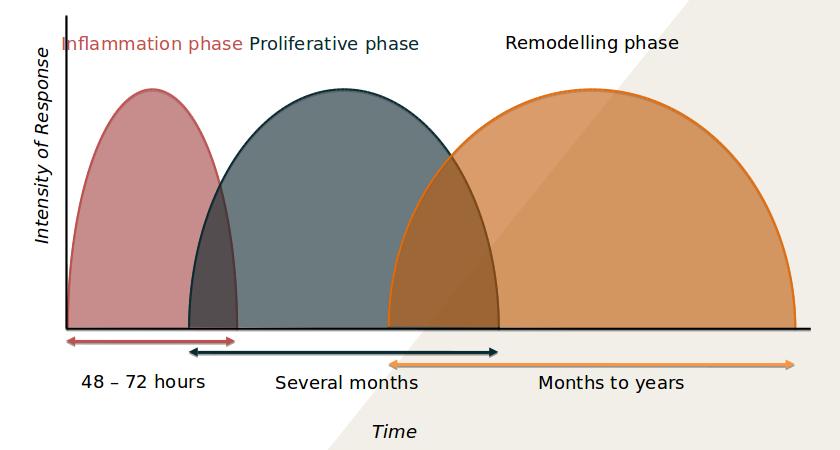
Difference following Healing
| Normal ligaments | Healed ligaments |
|---|---|
| Larger collagen fibrils | Smaller collagen fibrils |
| Low cell and matrix turnover | High cell and matrix turnover |
| Aligned collagen | Disorganised collagen |
| Densely packed collagen | Flaws between fibres |
| Higher matrix-cell ratio | Lower matrix-cell ratio |
| Low cell density | Higher cell density |
| Mature collagen cross-links | Immature collagen cross-links |
| Primarily collagen Type I | More collagen III |
| Primarily small proteoglycans | Larger proteoglycans |
| Rare cell division | More cell division |
Is it all about the ligaments?
Tenderness along Peroneal tendon common in acute sprains (Nelson & Rottman, 2007)
Reported muscle weakness/ altered muscle activity in those with ankle sprain history
Cartilage damage and osteochondral defects - Evidence after an acute/ recurrent sprains
Prevention
Factors we can change
| Non-modifiable | Modifiable |
|---|---|
| Sex | Weight |
| Age | BMI |
| Height | Neuromuscular control |
| Race | Postural stability |
| Foot/ ankle anatomy | Muscle strength |
| Extremity alignemtn | Exposure to sport |
| Previous ankle sprain | Player position |
| Generalised joint laxity | Footwear |
| Playing surface | |
| Skill level |
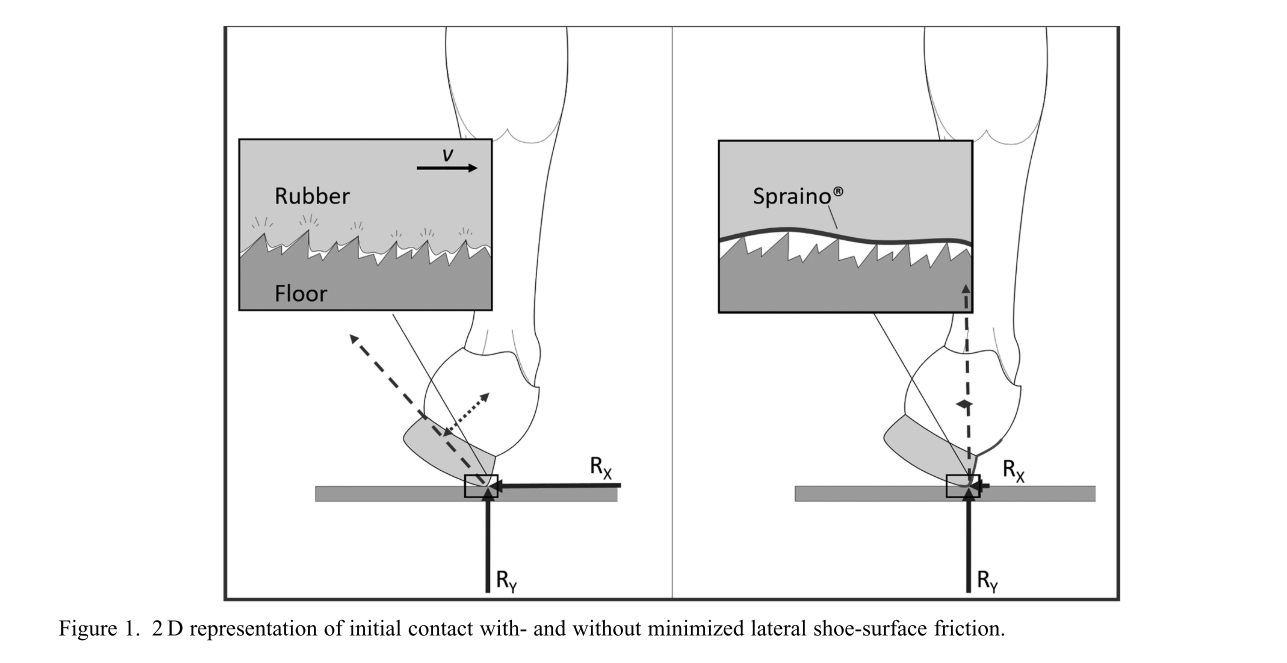
New Footwear
- Spraino
- Reduces shear force to allow sliding
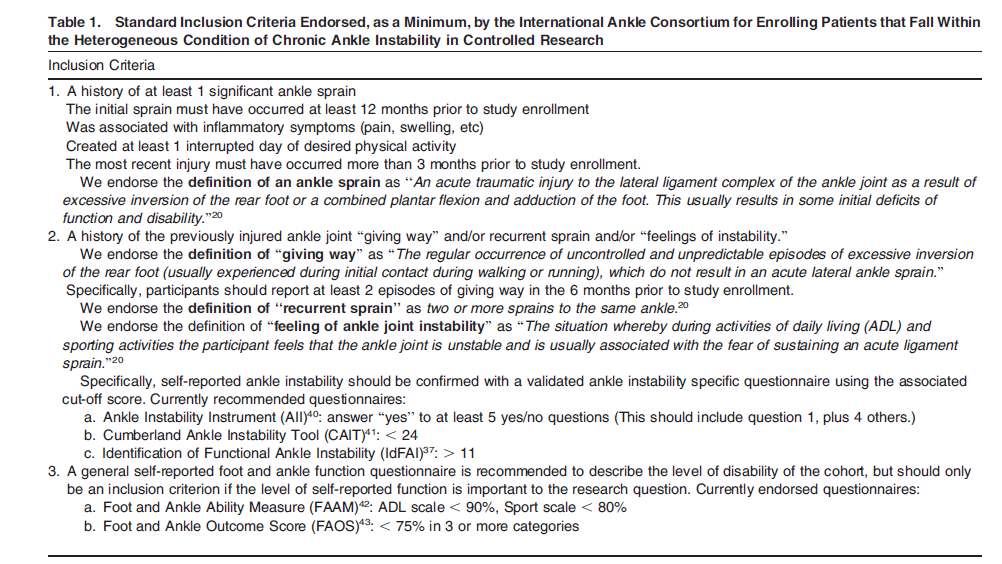
Chronic Ankle Instability
Gribble et al. (2014)
Pathomechanical Impairments
Hertel & Corbett (2019)
- Tissue adaptation
- Pathologic laxity
- Arthrokinematic restrictions
- Osteokinematic restrictions
- Secondary tissue injury
Sensory-Perceptual Impairments
Hertel & Corbett (2019)
- Pain
- Diminished somatosensation
- Perceived instability
- Kinesiophobia - Relates to the fear of movement or reinjury during functional activities.
- Reduced health-related QoL
- Lower self-reported function
Motor-Behavioural Impairments
Hertel & Corbett (2019)
- Altered reflexes
- Neuromuscular inhibition
- Balance deficits
- Reduced physical activity
- Muscle weakness
- Ankle evertors/ invertors and plantar flexors
- Hip abductors/ extensors/ external rotators
- Knee flexors/ extensors
- Altered movement patterns
- Employs a hip strategy ↑ flexion ↓ abduction
- ↓ Ankle DF ROM
- Inverted/ everted ankle at landing
- ↑ Knee flexion/↓ Knee flexion
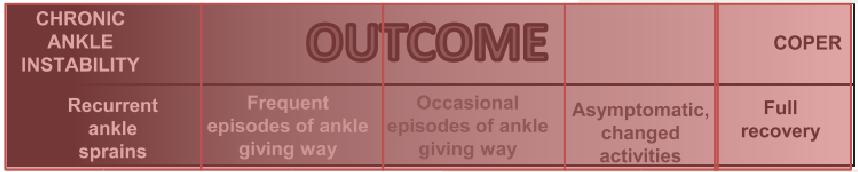
Outcome
Different presentation of impairments
Ideally, an ankle sprain patient becomes a Coper without changing their activity
Currently, unclear what causes an individual to become a coper/ CAI individual
Minimising re-injury in the CAI Population
1. Lace-up Braces

Theoretical Effects
Reduce swelling
Restrict ankle motion
- Provide mechanical resistance to inversion
- Hall et al., 2016 = restricted inversion ROM, reduced maximum inversion, reduced inversion velocity
Benefits
- Protect against inversion – aid in promoting proper collagen fibre orientation
- Useful during proliferation phase
Experimental Results
Found to reduce muscle activity during rehabilitation exercises (Feger et al., 2016)
- Reduced peroneal longus activity
- Aid in foot ankle alignment during weight bearing tasks
- Potentially reduces reliance on peroneals to control motion
- Mechanical support could be counter productive (long term use)?
2. Taping
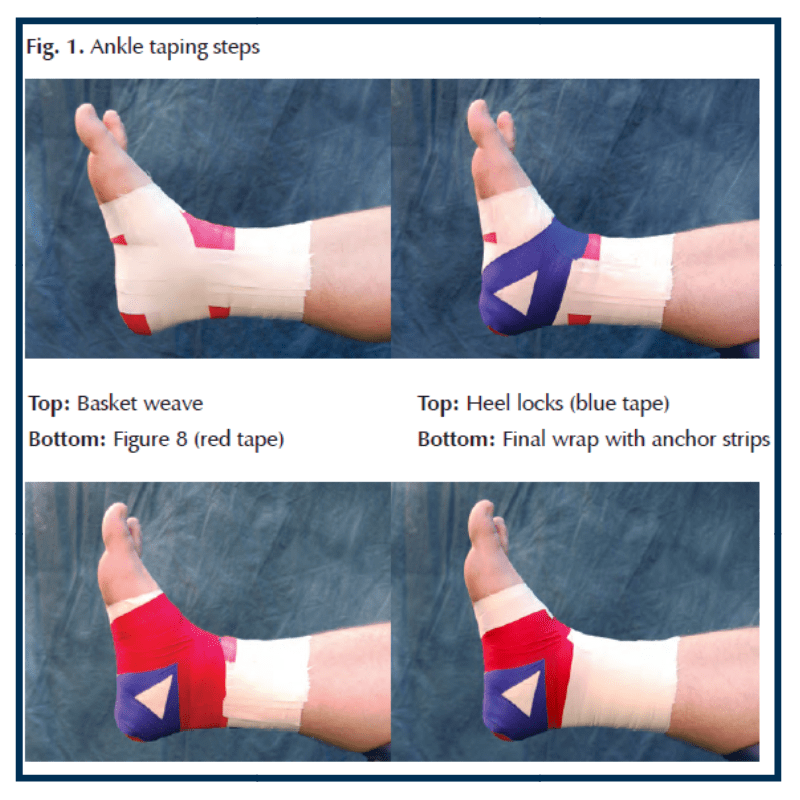
Theoretical Effects
Provides support and proprioceptive feedback?
- Limited evidence to support improve proprioception
Improve self efficacy
- Improved perceptions of stability, confidence and reassurance (Delahunt et al., 2010; Halim-Kertanegara et al., 2017)
Benefits
- Does not affect performing e.g. jumping performance
Issues
- Requires experience in taping
- Not user friendly
3. Semi-Rigid Braces

Theoretical Effects
- Provides some support to the ankle
- Improves postural control (Hadadi et a;., 2011; Maeda et al., 2016)
- Improved JPS
Benefits
- Improved proprioception
- Stimulation of skin
- Greater input to cutaneous mechanoreceptors
- Enhances feedback
Summary
- Lateral ankle sprains are common in sport
- Damage occurs to the ligaments and other structures around the ankle which requires time for healing
- Chronic ankle instability occurs in a high proportion of individuals following an acute sprain which can lead to long term consequences
- Impairments include – pathomechanical, sensory-perceptual and motor-behavioural
- Braces and taping can provide a range of support, resistance to movement and proprioceptive feedback to prevent recurrent sprains
References
Abdeen, R., Comfort, P., Starbuck, C., & Nester, C. (2018). Ultrasound Characteristics of Foot and Ankle Structures in Healthy, Coper and Chronically Unstable Ankles. Journal of Ultrasound in Medicine, 1–10. http://doi.org/10.1002/jum.14770
Burcal, C. J., & Wikstrom, E. A. (2016). Plantar Cutaneous Sensitivity With and Without Cognitive Loading in People With Chronic Ankle Instability, Copers, and Uninjured Controls. Journal of Orthopaedic & Sports Physical Therapy, 46(4), 270–276. http://doi.org/10.2519/jospt.2016.6351
Burks, R. T., & Morgan, J. (1998). Anatomy of the lateral ankle ligaments. The American Journal of Sports Medicine, 22(1), 72–7. http://doi.org/10.1177/036354659402200113
de Asla, R. J., Kozanek, M., Wan, L., Rubash, H. E., & Li, G. (2009). Function of anterior talofibular and calcaneofibular ligaments during in-vivo motion of the ankle joint complex. J Orthop Surg Res, 4, 7. http://doi.org/10.1186/1749-799X-4-7
Delahunt, E., McGrath, A., Doran, N., & Coughlan, G. F. (2010). Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Archives of Physical Medicine and Rehabilitation, 91(9), 1383–1389. http://doi.org/10.1016/j.apmr.2010.06.023
Doherty, C., Delahunt, E., Caulfield, B., Hertel, J., Ryan, J., & Bleakley, C. (2014). The Incidence and Prevalence of Ankle Sprain Injury: A Systematic Review and Meta-Analysis of Prospective Epidemiological Studies. Sports Medicine, 44(1), 123–140. http://doi.org/10.1007/s40279-013-0102-5
Feger, M. A., Donovan, L., Hart, J. M., & Hertel, J. (2014). Effect of ankle braces on lower extremity muscle activation during functional exercises in participants with chronic ankle instability. International Journal of Sports Physical Therapy, 9(4), 476–87. http://doi.org/10.1016/j.ptsp.2014.02.002
Fong, D. T. P., Ha, S. C. W., Mok, K. M., Chan, C. W. L., & Chan, K. M. (2012). Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: Five cases from televised tennis competitions. American Journal of Sports Medicine, 40(11), 2627–2632. http://doi.org/10.1177/0363546512458259
Fong, D. T. P., Hong, Y., Shima, Y., Krosshaug, T., Yung, P. S. H., & Chan, K. M. (2009). Biomechanics of supination ankle sprain: A case report of an accidental injury event in the laboratory. American Journal of Sports Medicine, 37(4), 822–827. http://doi.org/10.1177/0363546508328102
Gehring, D., Wissler, S., Mornieux, G., & Gollhofer, A. (2013). How to sprain your ankle - a biomechanical case report of an inversion trauma. Journal of Biomechanics, 46(1), 175–178. http://doi.org/10.1016/j.jbiomech.2012.09.016
Gribble, P. A., Bleakley, C. M., Caulfield, B. M., Docherty, C. L., Fourchet, F., Fong, D. T.-P., … Delahunt, E. (2016). Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. British Journal of Sports Medicine, 24, 1496–1505. http://doi.org/10.1136/bjsports-2016-096189
Gribble, P. A., Delahunt, E., Bleakley, C. M., Caulfield, B., Docherty, C. L., Fong, D. T. P., … Wikstrom, E. A. (2014). Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the international ankle consortium. Journal of Athletic Training, 49, 121–127. http://doi.org/10.4085/1062-6050-49.1.14
Hadadi, M., Mazaheri, M., Mousavi, M. E., Maroufi, N., Bahramizadeh, M., & Fardipour, S. (2011). Effects of soft and semi-rigid ankle orthoses on postural sway in people with and without functional ankle instability. Journal of Science and Medicine in Sport, 14(5), 370–375. http://doi.org/10.1016/j.jsams.2010.12.004
Halim-Kertanegara, S., Raymond, J., Hiller, C. E., Kilbreath, S. L., & Refshauge, K. M. (2017). The effect of ankle taping on functional performance in participants with functional ankle instability. Physical Therapy in Sport, 23, 162–167. http://doi.org/10.1016/j.ptsp.2016.03.005
Hall, E. A., Simon, J. E., & Docherty, C. L. (2016). Using ankle bracing and taping to decrease range of motion and velocity during inversion perturbation while walking. Journal of Athletic Training, 51(4), 283–290. http://doi.org/10.4085/1062-6050-51.5.06
Hauser, R., & Dolan, E. (2011). Ligament Injury and Healing : An Overview. Journal of Prolotherapy, 3(4), 836–846. http://doi.org/10.1002/14651858.CD003762
Hertel, J., & Corbett, R. O. (2019). An Updated Model of Chronic Ankle Instability. Journal of Athletic Training, 54(6), 1062-6050-344–18. http://doi.org/10.4085/1062-6050-344-18
Hootman, J. M., Dick, R., & Agel, J. (2007). Epidemiology of collegiate injuries for 15 sports: Summary and recommendations for injury prevention initiatives. Journal of Athletic Training.
Houston, M. N., Van Lunen, B. L., & Hoch, M. C. (2014). Health-related quality of life in individuals with chronic ankle instability. Journal of Athletic Training, 49(6), 758–763. http://doi.org/10.4085/1062-6050-49.3.54
Lobo, C. C., Morales, C. R., Sanz, D. R., Corbalán, I. S., Marín, A. G., & López, D. L. (2016). Ultrasonography Comparison of Peroneus Muscle Cross-sectional Area in Subjects With or Without Lateral Ankle Sprains. Journal of Manipulative and Physiological Therapeutics, 39, 635–644. http://doi.org/10.1016/j.jmpt.2016.09.001
Lysdal, F. G., Jakobsen, L., Grønlykke, T. B., & Kersting, U. (2019). A kinematic analysis of the Spraino® realignment mechanism during simulated noncontact ankle sprain injuries. Footwear Science, 11(sup1), S167–S169. http://doi.org/10.1080/19424280.2019.1606309
Maeda, N., Urabe, Y., Tsutsumi, S., Numano, S., Morita, M., Takeuchi, T., … Kobayashi, T. (2016). Effect of semi-rigid and soft ankle braces on static and dynamic postural stability in young male adults. Journal of Sports Science and Medicine, 15(2), 352–357.
McCriskin, B. J., Cameron, K. L., Orr, J. D., & Waterman, B. R. (2015). Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World Journal of Orthopedics, 6(2), 161–71. http://doi.org/10.5312/wjo.v6.i2.161
Nie, B., Panzer, M. B., Mane, A., Mait, A. R., Donlon, J. P., Forman, J. L., & Kent, R. W. (2017). Determination of the in situ mechanical behavior of ankle ligaments. Journal of the Mechanical Behavior of Biomedical Materials, 65, 502–512. http://doi.org/10.1016/j.jmbbm.2016.09.010
Pavailler, S., & Horvais, N. (2014). Sliding Allows Faster Repositioning during Tennis Specific Movements on Hard Court. Procedia Engineering, 72(72), 859–864. http://doi.org/10.1016/j.proeng.2014.06.157
Pavailler, S., & Horvais, N. (2015). Trunk and lower limbs muscular activity during tennis-specific movements: effect of sliding on hard and clay court. Footwear Science, 7(sup1), S68–S70. http://doi.org/10.1080/19424280.2015.1038612
Rochelle, D. C., Herbert, A., Ktistakis, I., Redmond, A. C., Chapman, G. J., & Brockett, C. L. (2020). Mechanical characterisation of the lateral collateral ligament complex of the ankle at realistic sprain-like strain rates. Journal of the Mechanical Behavior of Biomedical Materials, 102(September 2019), 103473. http://doi.org/10.1016/j.jmbbm.2019.103473
Roos, K. G., Kerr, Z. Y., Mauntel, T. C., Djoko, A., Dompier, T. P., & Wikstrom, E. A. (2017). The Epidemiology of Lateral Ligament Complex Ankle Sprains in National Collegiate Athletic Association Sports. The American Journal of Sports Medicine, 45(1), 201–209. http://doi.org/10.1177/0363546516660980
Sakai, S., Urabe, Y., Morikawa, M., Fujishita, H., Komiya, M., Sasadai, J., … Maeda, N. (2018). Quantity and quality of the peroneus longus assessed using ultrasonography in leg with chronic ankle instability. Journal of Physical Therapy Science, 30(12), 1396–1400. http://doi.org/10.1589/jpts.30.1396
Wikstrom, E. A. (2011). Fear of re-injury does not differ between those with and without chronic ankle instability. Journal of Sports Science and Medicine, 10(4), 771–772.