Public Health Strategies
Definitions
Expand
Health
‘a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and physical resources, as well as capabilities’ (Ottowa Charter for Health Promotion, 1986) – see http://www.who.int/healthpromotion/conferences/previous/ottawa/en/
Public Health
Public health is a social and political concept aimed at the improving health, prolonging life and improving the quality of life among whole populations through health promotion, disease prevention and other forms of health intervention. http://www.who.int/healthpromotion/about/HPG/en/
Free will
Health is a choice based on decisions taken by individuals affecting behaviour and lifestyle
Determination
Health is determined by external factors outside your control
- This debate is important, because it affects how we attempt to deal with health issues nationally and globally.
- e.g if you believe that poor nutrition or physical inactivity is based on ‘free will’, then you can use health education campaigns in order to change people’s behaviour
- However, if you believe that poor nutrition or physical inactivity is determined largely by socio-cultural and political influences, then you may wish to create policies that help people’s nutrition/physical activity to improve –
- e.g. subsidising certain foods – policies to reduce sugar/salt in certain foods or investing in local and parks/leisure facilities and creating policies to increase PA in schools
Lifestyle vs behaviour
Expand
“If behaviour is understood within a complex web that makes up a lifestyle, it immediately becomes evident that attempts to change the behavior will need to have regard for the social, environmental and cultural circumstances that sustain that lifestyle” (Green & Tones, 2010, p.86).
“If behaviour is understood within a complex web that makes up a lifestyle, it immediately becomes evident that attempts to change the behavior will need to have regard for the social, environmental and cultural circumstances that sustain that lifestyle” (Green & Tones, 2010, p.86).
5 Major Determinants of Health
Expand
Biological factors
Lifestyle
Environment
Social & Environmental factors
- ‘probably the most powerful known influences on population health…[t]wo, three, or even four-fold mortality differences have been reported between groups of high and low status (Wilkinson 1999 p.528).
The use of and access to health services
Health Inequality/Inequity
Expand
Health inequalities can be defined as differences in health status or in the distribution of health determinants between different population groups.
Some health inequalities are attributable to biological variations or free choice and others are attributable to the external environment and conditions mainly outside the control of the individuals concerned.
Health inequities – unfair, unjust and avoidable causes of ill health
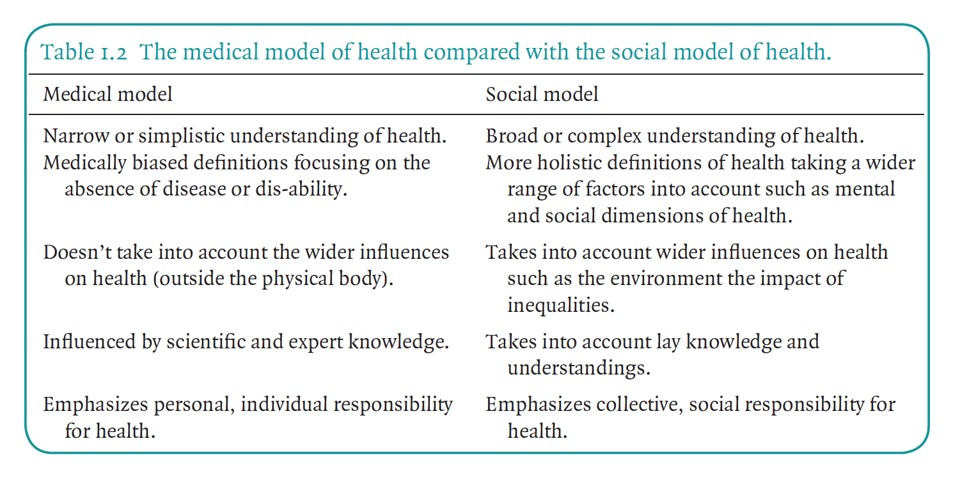
2 Main Health Models
Expand
UK Faculty of Public Health
Expand
The Faculty’s approach is that public health: - is population based - emphasises collective responsibility for health, its protection and disease prevention - recognises the key role of the state, linked to a concern for the underlying socio-economic and wider determinants of health, as well as disease - emphasises partnerships with all those who contribute to the health of the population.
Health Promotion
Expand
“Health promotion is the process of enabling people to increase control over, and to improve their health” Health Promotion Glossary, WHO (1998)
Health promotion encompasses health education, but also includes action at the social and political level to influence the environments within which individuals and groups live and work. At its simplest, it is anything that contributes to health improvement
Public Health has much in common with Health Promotion in that they are largely focused on population health. They both have roots in the international debates around the promotion of health in the 1970/80s, and are both underpinned by the WHO Health for All principles.
Public Health can be viewed as a broader top-down approach, whereas Health Promotion is one aspect of Public Health.
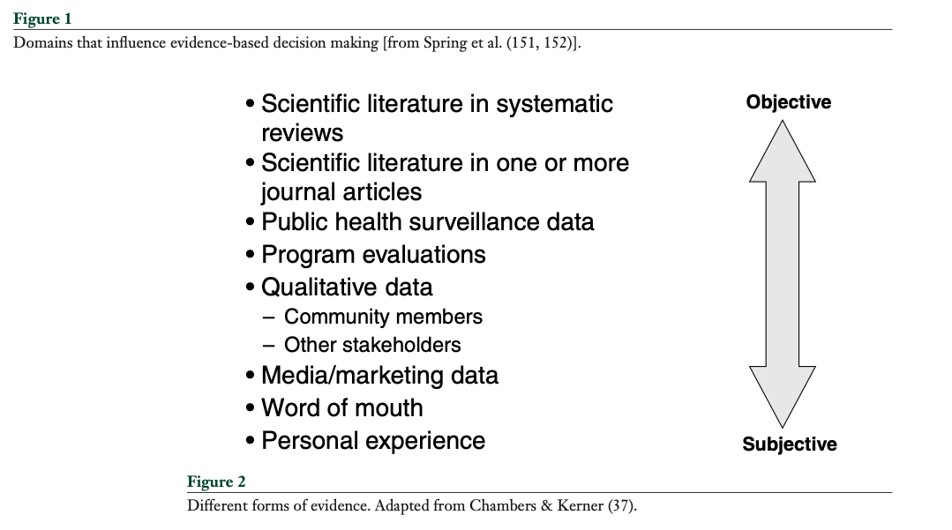
Evidence Based Public Health
Expand
“EBPH can be defined as a process of integrating evidence from scientific research and practice to improve the health of the target population” (Vagagas, Bala & Lhachimi, 2017).
“An EBPH approach could potentially have numerous direct and indirect benefits, including access to more and higher-quality information on best practice, a higher likelihood of successful prevention programs and policies, greater workforce productivity, and more efficient use of public and private resources” (ibid).
‘integrating science-based interventions with community preferences for improving population health’
Challenges with EBPH
Expand
Absence of evidence
Knowing how much evidence is enough to judge and evaluate policy decisions
Lots of evidence about what needs to be done, but far less about what and how to do it
Type 1 evidence defines the causes of diseases and the magnitude, severity, and preventability of risk factors and diseases. It suggests that “something should be done” about a particular disease or risk factor.
Type 2 evidence describes the relative impact of specific interventions that do or do not improve health, adding “specifically, this should be done”
Type 3 evidence (of which we have the least) shows how and under which contextual conditions interventions were implemented and how they were received, thus informing “how something should be done”
Levels of Intervention
Expand
Strengthening individuals: (person based strategies to improved the health of disadvantaged individuals
Strengthening communities: (improving the health of disadvantaged communities and local areas by building social cohesion and mutual support
Improving living and working conditions: (reducing exposure to health-damaging environments across the whole population)
Promoting healthy macro policy: (improving the macro-economic, cultural and environmental context which influence the standard of living achieved by the whole population)
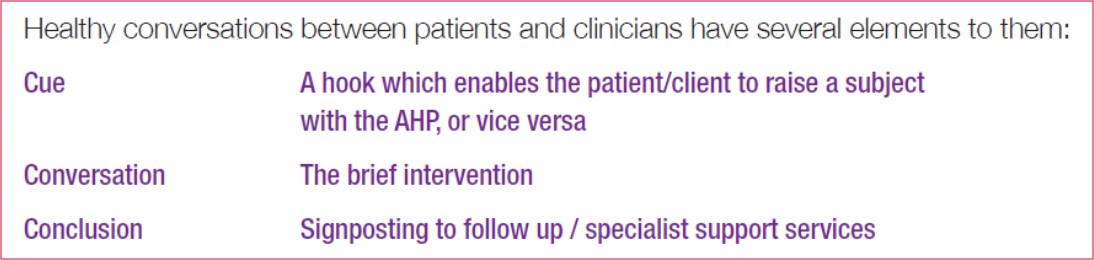
Healthy Conversation Approach
Expand
- Often termed MECC (Making Every Contact Count)
- A ‘healthy’ conversation occurs opportunistically and involves an individual being encouraged to consider their lifestyle and health with a view to identifying small but important services.
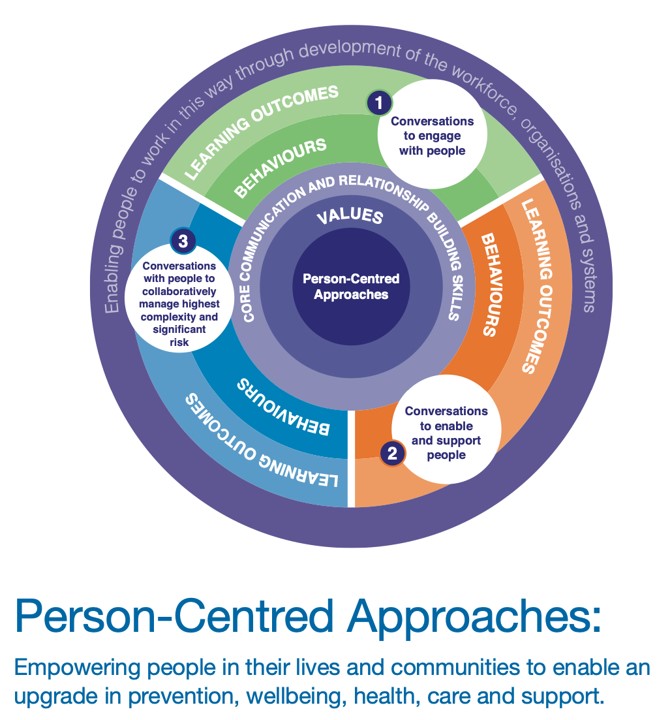
Person Centred Approaches
Expand
A person-centred approach puts people, families and communities at the heart of health, care and wellbeing
a person-centred approach is about being ‘community focussed’ i.e. seeing the person in the context of their whole life and recognising that the most appropriate activity, treatment or support may be community based.
Growing body of evidence (e.g. Realising the Value [2016] research and the National Voices Evidence for Person Centred Care [2017]) that it can lead to better outcomes and care for people and make better use of finite resources. Crucially, this approach is also now the focus of policy and legislation, notably the Five Year Forward View (Chapter 2), which emphasises the aim for ‘a more engaged relationship with patients, carers and citizens so that we can promote wellbeing and prevent ill-health’, together with the Care Act (2014) which aims to put people at the centre of their care and support and maximise their involvement.
Tools and Resources for EBPH
Expand
See – Jacobs et al (2012) - http://www.cdc.gov/pcd/issues/2012/11_0324.htm
EXCELLENT PAPER - Evidence-Based Public Health: A Fundamental Concept for Public Health Practice https://www.annualreviews.org/doi/pdf/10.1146/annurev.publhealth.031308.100134
EXCELLENT PAPER - A glossary for evidence based public health - https://jech.bmj.com/content/58/7/538.short
Evidence-based public health: what does it offer developing countries? - https://academic.oup.com/jpubhealth/article/27/2/215/1595882